How to fix a failed cervical fusion? Well, it’s not quite as simple as replacing a broken vase, but we’re here to demystify this potentially tricky medical situation. This comprehensive guide delves into the complexities of failed cervical fusions, from the initial diagnosis to the long-term outlook. Get ready to navigate the world of surgical and non-surgical interventions, and discover the surprising ways to get back on track.
Cervical fusion, a procedure that aims to stabilize the neck, can sometimes encounter setbacks. Factors like the type of fusion, patient characteristics, and the presence of complications can influence the outcome. This article provides a detailed breakdown of the various stages involved in addressing a failed cervical fusion, offering insights into diagnosis, treatment options, and post-operative care. This isn’t your typical medical textbook; it’s a friendly guide to understanding this intricate process.
Introduction to Cervical Fusion Failure
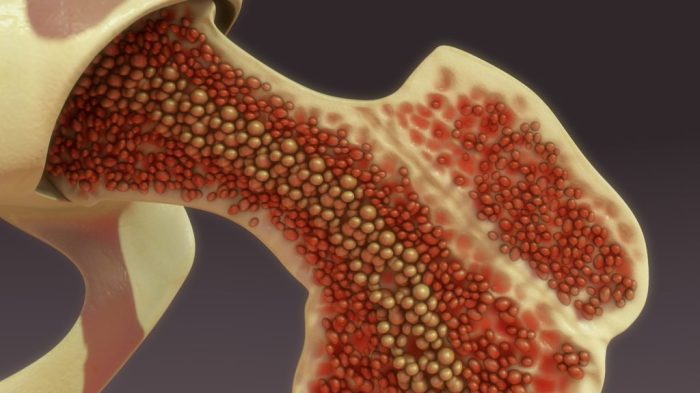
Cervical fusion is a surgical procedure used to stabilize the spine in the neck region. This procedure aims to alleviate pain and improve function by fusing together two or more vertebrae. It’s a common treatment for conditions like degenerative disc disease, herniated discs, and spinal stenosis, but like any surgical intervention, it carries the potential for complications. Understanding the factors that contribute to fusion failure is crucial for patients and healthcare professionals alike.A cervical fusion might fail due to various reasons.
These include inadequate bone graft integration, infection, improper alignment of the vertebrae, or persistent movement at the fusion site. Other factors that can increase the risk of failure include pre-existing medical conditions, smoking, poor patient compliance with post-operative instructions, and even the type of fusion procedure itself. Understanding the nuances of each procedure type is essential for a comprehensive understanding of possible failure points.
Common Reasons for Cervical Fusion Failure
A failed cervical fusion can stem from a variety of factors. Inadequate bone graft integration, where the bone graft fails to properly fuse with the vertebrae, is a frequent cause. Poor surgical technique, leading to improper alignment or insufficient fusion, can also result in failure. Infection at the fusion site, a rare but serious complication, can impede the healing process and disrupt the fusion.
Furthermore, persistent movement at the fusion site can create instability and pain.
Types of Cervical Fusion Procedures and Potential Failure Points
Different surgical approaches are used for cervical fusion. Each approach has its own potential complications and failure points.
| Procedure Type | Potential Complications | Risk Factors | Treatment Options |
|---|---|---|---|
| Anterior Cervical Discectomy and Fusion (ACDF) | Potential for damage to the recurrent laryngeal nerve, esophagus, or trachea; infection, implant loosening, nonunion, adjacent segment disease, and persistent pain. | Smoking, poor bone quality, pre-existing medical conditions, and patient age are some factors. | Revision surgery, pain management, physical therapy, and potentially a different fusion approach. |
| Posterior Cervical Fusion | Potential for damage to the spinal cord, nerves, or blood vessels; infection, nonunion, adjacent segment disease, and persistent pain. | Patient age, bone quality, and pre-existing medical conditions. | Revision surgery, pain management, physical therapy, and possibly a different fusion approach. |
Symptoms of a Failed Cervical Fusion
Symptoms of a failed cervical fusion can vary, but they often involve persistent neck pain, stiffness, or discomfort. Neurological symptoms, such as numbness, tingling, or weakness in the arms or hands, can also occur. Furthermore, patients might experience headaches or difficulty with swallowing or breathing. These symptoms may not appear immediately after surgery and can manifest months or even years later.
Diagnosis and Evaluation of Failed Fusion
Successfully diagnosing a failed cervical fusion requires a multifaceted approach, combining meticulous clinical evaluation with advanced imaging techniques. Accurate diagnosis empowers healthcare professionals to develop the most appropriate and personalized treatment plan, ultimately optimizing patient outcomes and minimizing the impact of the failed procedure. This meticulous process is critical for successful management and restoration of optimal cervical function.A thorough understanding of the diagnostic methods used in evaluating a failed cervical fusion is essential.
This includes a comprehensive evaluation of imaging studies, meticulous clinical examination, and detailed patient history. Each piece of information contributes to a complete picture of the patient’s condition, allowing for a precise diagnosis and a tailored treatment strategy.
Imaging Techniques
Accurate diagnosis of a failed cervical fusion hinges on a careful analysis of various imaging techniques. These methods provide crucial insights into the structural integrity of the spine, the presence of complications, and the overall status of the fusion site.X-rays, CT scans, and MRI scans are commonly utilized in assessing cervical spine conditions, each with unique strengths and weaknesses.
These techniques offer different perspectives of the affected area, facilitating a more complete picture of the condition and guiding treatment decisions. Radiographic imaging is pivotal in this process, providing detailed information for both the surgeon and the patient.
Clinical Examination and Patient History
Clinical examination and patient history are essential components of the diagnostic process for a failed cervical fusion. A detailed clinical examination allows healthcare professionals to assess the patient’s current neurological status, range of motion, and pain levels. The patient’s subjective experience, including details about the onset, duration, and characteristics of the pain, is equally important.A thorough patient history, encompassing previous treatments, medications, and any relevant medical conditions, aids in understanding the complete clinical picture.
This detailed history can provide invaluable context for interpreting imaging results and formulating an effective treatment plan. Gathering detailed patient input about their symptoms and past treatments is essential.
Diagnostic Imaging Comparison
| Imaging Technique | Strengths | Weaknesses | Applications |
|---|---|---|---|
| X-ray | Excellent for visualizing bone structure and alignment, relatively inexpensive, and readily available. | Limited soft tissue visualization, less detailed than CT or MRI, may not detect subtle bony abnormalities. | Initial screening for alignment issues, follow-up on fusion progress, assessing for post-operative complications like displacement or loosening. |
| CT Scan | Excellent for visualizing bony structures in great detail, good at detecting fractures, bone loss, or hardware malposition. Can provide cross-sectional views, which are useful for evaluating complex regions. | Limited soft tissue visualization, higher radiation exposure compared to X-ray, may not be ideal for assessing neural structures. | Detailed evaluation of bony anatomy, identifying fractures, assessing the status of the fusion mass, evaluating for hardware loosening or migration, evaluating bone loss or defects. |
| MRI | Excellent for visualizing soft tissues, including nerves, ligaments, and discs, highly sensitive to subtle changes in soft tissue and inflammation. | Longer scanning time, may not be as readily available as X-rays or CT scans, more expensive, and potential contraindications for patients with certain medical devices or implants. | Assessing for nerve impingement, identifying disc herniations or soft tissue abnormalities in the cervical spine, identifying inflammation or scarring at the fusion site, evaluating for any soft tissue complications, and evaluating for any post-operative complications. |
Treatment Options for Failed Cervical Fusion
Restoring optimal cervical spine function after a failed fusion is a multifaceted endeavor. Understanding the diverse treatment options available is crucial for navigating this complex process. Careful consideration of individual patient factors, surgical history, and desired outcomes will ultimately guide the selection of the most appropriate course of action.Comprehensive assessment and personalized strategies are paramount in addressing the unique challenges posed by failed cervical fusions.
The goal is to minimize pain, improve mobility, and enhance overall quality of life. Success hinges on a thorough understanding of the failure’s cause, the patient’s specific needs, and the potential benefits and risks of each available approach.
Surgical Treatment Approaches
Surgical interventions for failed cervical fusions aim to address the underlying cause of the problem, potentially restoring spinal stability and relieving symptoms. Different surgical techniques are employed depending on the nature of the failure and the patient’s individual circumstances. Careful consideration of potential risks and benefits is essential in making informed decisions.
| Treatment Approach | Procedures | Success Rate | Risks |
|---|---|---|---|
| Revision Cervical Fusion | Re-operating to correct the original fusion, potentially using different techniques or materials, to achieve a stable and functional fusion. This may include addressing bony defects, removing fibrous tissue, and re-establishing proper alignment. | Studies show variable success rates, often ranging from 60-80% depending on the specific cause of failure and the skill of the surgeon. | Risks include infection, bleeding, nerve damage, hardware failure, and the potential for further complications from the initial fusion procedure. A skilled and experienced surgeon minimizes these risks. |
| Laminoplasty | A surgical technique that creates a window in the lamina (the bony arch of the vertebra) to relieve pressure on the spinal cord or nerves. This may be a suitable option for patients with stenosis or impingement. | Success rates for laminoplasty in revision cases are generally good, with outcomes often exceeding 70%. | Risks include infection, bleeding, nerve damage, and the potential for complications related to the creation of the window in the lamina. Post-operative pain and stiffness are also possible. |
| Anterior Cervical Discectomy and Fusion (ACDF) Revision | Re-performing ACDF to address the failure of the initial procedure. This involves removing the damaged disc and replacing it with a bone graft and/or implant, allowing for healing and stabilization. | Success rates for revision ACDF can vary but often fall within the 70-90% range if performed by experienced surgeons. | Risks include infection, bleeding, nerve damage, implant loosening or breakage, and the potential for recurrent problems. |
Non-Surgical Treatment Approaches
Non-surgical interventions are often considered as initial treatment options or as complementary therapies alongside surgical interventions.
| Treatment Approach | Procedures | Success Rate | Risks |
|---|---|---|---|
| Physical Therapy | Exercises and stretches tailored to address neck pain, improve range of motion, and strengthen supporting muscles. | Studies suggest that physical therapy can be effective in managing pain and improving function in some cases, but success depends on adherence to the program and the severity of the problem. | Risks are generally low, but potential for worsening pain if not performed properly or if the patient is not compliant. |
| Medications | Pain relievers, anti-inflammatory drugs, and muscle relaxants can help manage pain and discomfort. In some cases, steroid injections may be considered. | Medications can provide temporary relief, but they may not address the underlying cause of the failed fusion. Success depends on the type and severity of the condition. | Risks associated with medications can include side effects such as nausea, stomach upset, or interactions with other medications. Steroid injections carry risks of infection, nerve damage, or bleeding. |
| Cervical Collar/Bracing | Wearing a supportive collar or brace can help immobilize the neck and reduce pain. | This approach may offer temporary relief, but it may not address the root cause of the failed fusion. | Risks include discomfort and potential for skin irritation. Long-term use can lead to muscle weakness and stiffness if not managed properly. |
Factors Influencing Treatment Choice
The selection of the optimal treatment strategy depends on various factors, including the cause of the failed fusion, the patient’s overall health, and their preferences. Careful evaluation and collaboration between the patient and healthcare team are essential to ensure the most suitable path forward.
Post-operative Care and Rehabilitation

Successfully navigating the post-operative phase is crucial for a positive outcome after a cervical fusion. A comprehensive rehabilitation program, tailored to individual needs, significantly impacts recovery and long-term well-being. This phase focuses on restoring function, managing pain effectively, and preventing complications, ultimately empowering patients to regain their quality of life.
Importance of Post-operative Care
Rigorous post-operative care is vital for successful recovery and achieving the best possible outcome after a cervical fusion. It encompasses a multifaceted approach that includes diligent pain management, precise physical therapy, and proactive monitoring of potential complications. A personalized plan, designed in consultation with a healthcare team, is essential for a smooth and effective recovery.
Physical Therapy and Rehabilitation Programs
Structured physical therapy programs are essential for restoring strength, range of motion, and flexibility in the neck and surrounding areas. These programs typically involve a combination of exercises, manual therapy, and patient education. Early intervention and consistent adherence to the program are key to optimal recovery.
Pain Management Strategies
Effective pain management is paramount during the recovery period. A multi-modal approach, often including medication, physical therapy techniques, and lifestyle modifications, is frequently employed. This comprehensive strategy aims to minimize pain and discomfort, allowing patients to actively participate in rehabilitation and daily activities.
Potential Complications During Recovery, How to fix a failed cervical fusion
While cervical fusion is a generally safe procedure, potential complications can arise during the recovery period. These can include infection, persistent pain, stiffness, and nerve damage. Proactive monitoring and prompt intervention are essential to address these complications should they arise. Recognizing early warning signs and communicating them to the healthcare team is crucial.
Exercises and Activities for Rehabilitation
Incorporating a variety of exercises and activities into the rehabilitation program is essential for regaining strength, flexibility, and range of motion in the neck and surrounding areas. These activities should be gradually introduced and progressed as tolerated. A physical therapist can create a personalized exercise plan to meet individual needs and ensure safety.
- Gentle Neck Stretches: These are crucial for regaining flexibility and reducing stiffness. Examples include chin tucks, neck rotations, and side bends. These exercises should be performed slowly and carefully, avoiding any sudden or forceful movements.
- Range-of-Motion Exercises: These exercises help to restore the full range of motion in the neck. Exercises like shoulder rotations and arm circles can also be beneficial to improve overall mobility.
- Strengthening Exercises: These exercises gradually build strength in the neck muscles. Examples include isometric exercises and exercises using resistance bands. It is essential to gradually increase the intensity and duration of these exercises to avoid strain.
- Postural Exercises: Correct posture is crucial for long-term recovery. These exercises focus on maintaining good posture during daily activities, reducing stress on the neck and preventing further complications.
- Aerobic Exercises: Low-impact aerobic exercises, such as walking or swimming, are beneficial for overall health and well-being. These exercises can help improve cardiovascular health and increase energy levels.
Long-Term Outcomes and Prognosis
The journey toward recovery after a cervical fusion, even one that has encountered complications, is often a testament to the human spirit’s resilience and determination. Understanding the long-term outcomes, both positive and challenging, empowers individuals and their support systems to navigate this process with realistic expectations and a proactive approach to well-being. A clear understanding of potential outcomes helps in making informed decisions about treatment strategies and long-term management.
Factors Influencing Long-Term Success
Numerous factors influence the long-term success of cervical fusion procedures, and these are essential to consider in both the preoperative and postoperative stages. The initial health of the cervical spine, the severity of the underlying condition, the surgical technique, and the patient’s commitment to post-operative care all play a role in determining the outcome. Proper patient selection, meticulous surgical technique, and a strong support system contribute to the likelihood of positive long-term results.
For example, patients with a history of smoking or poor nutrition may experience slower healing and reduced success rates.
Successful Outcomes
Many individuals experience significant improvement in their quality of life following treatment for a failed cervical fusion. Successful outcomes can manifest in reduced pain, improved range of motion, and a return to activities previously limited by neck pain. Examples include individuals who, after undergoing revision surgery or alternative treatments, regained the ability to work, participate in hobbies, and engage in daily activities without significant discomfort.
Such outcomes highlight the potential for positive change and underscore the importance of individualized treatment plans.
Unsuccessful Outcomes
While many patients experience positive results, some individuals may continue to experience persistent pain, reduced range of motion, or other complications. These outcomes can stem from factors such as the complexity of the original or revision surgery, the patient’s response to treatment, and the presence of co-morbidities. Careful evaluation of each patient’s specific needs and circumstances is critical in managing expectations and providing appropriate care.
For instance, patients with pre-existing neurological conditions may experience more persistent or severe symptoms, despite successful fusion.
Summary of Long-Term Outcomes
| Treatment Group | Success Rate | Complications | Quality of Life Improvement |
|---|---|---|---|
| Revision Surgery (e.g., fusion with instrumentation) | Generally higher than initial fusion in terms of pain reduction, but success rates vary significantly based on the underlying cause of failure and patient factors. | Potential for new complications from the revision surgery (e.g., nerve damage, infection, hardware failure) and the persistence of original issues. | Significant improvement in pain and function, but not always a complete return to pre-injury function. |
| Non-Surgical Interventions (e.g., physical therapy, medication) | Variable success rates, often less effective for severe cases. | Generally lower risk of complications compared to surgery. | May improve pain and function, but the extent of improvement is typically less than that seen with surgery. |
| Alternative Therapies (e.g., acupuncture, massage) | Limited scientific evidence supporting long-term efficacy. | Generally low risk of complications. | Potentially beneficial for symptom management and improving overall well-being, but typically not the primary treatment for failed fusion. |
Last Point: How To Fix A Failed Cervical Fusion
So, there you have it – a deep dive into the world of failed cervical fusions. We’ve covered everything from understanding the initial failure to exploring the diverse treatment approaches and the crucial role of post-operative care. Remember, every case is unique, and the best course of action depends on individual circumstances. While this guide provides a wealth of information, consulting with a qualified medical professional remains paramount for personalized guidance and optimal outcomes.
FAQ Insights
What are some common reasons why a cervical fusion might fail?
Several factors can contribute to fusion failure, including poor bone graft integration, infection, and underlying medical conditions. Sometimes, the initial fusion wasn’t properly performed in the first place, leaving room for the problem to resurface. It’s like trying to build a tower of cards – one misplaced card, and the whole thing collapses.
What are some non-surgical treatment options for a failed cervical fusion?
Non-surgical options might include physical therapy, medication management, and lifestyle adjustments to manage pain and improve neck function. Think of it as a gentler approach, similar to fine-tuning a car’s engine instead of completely rebuilding it.
How long does the recovery period typically last after a failed cervical fusion revision?
The recovery period after a failed cervical fusion revision can vary significantly depending on the complexity of the procedure and the individual’s response. It could range from a few weeks to several months. It’s like a marathon – some finish faster than others.
What are the long-term success rates for different treatment options for a failed cervical fusion?
Unfortunately, success rates for failed cervical fusion treatment aren’t universally published and depend heavily on the individual case. Factors like the underlying cause of the initial failure, the chosen treatment, and the patient’s overall health play a significant role. So, there’s no one-size-fits-all answer.
