How to release cluneal nerve pain? This guide dives deep into understanding, diagnosing, and managing this tricky pain. We’ll cover everything from the anatomy of the cluneal nerves to various treatment options, including lifestyle changes, physical therapy, and even potential surgical interventions. Get ready to conquer cluneal nerve pain!
Cluneal nerve pain can be a real pain in the neck, literally. This comprehensive guide breaks down the complexities of this condition, offering actionable steps to help you find relief. We’ll explore different types of pain, potential causes, and effective strategies for managing it.
Understanding Cluneal Nerve Pain
Cluneal nerve pain, often a source of discomfort and frustration, stems from irritation or damage to the cluneal nerves. These nerves, located in the lower back and buttock region, are responsible for sensation in the buttocks and surrounding areas. Understanding the intricacies of these nerves and the various factors contributing to their pain is crucial for effective management and treatment.
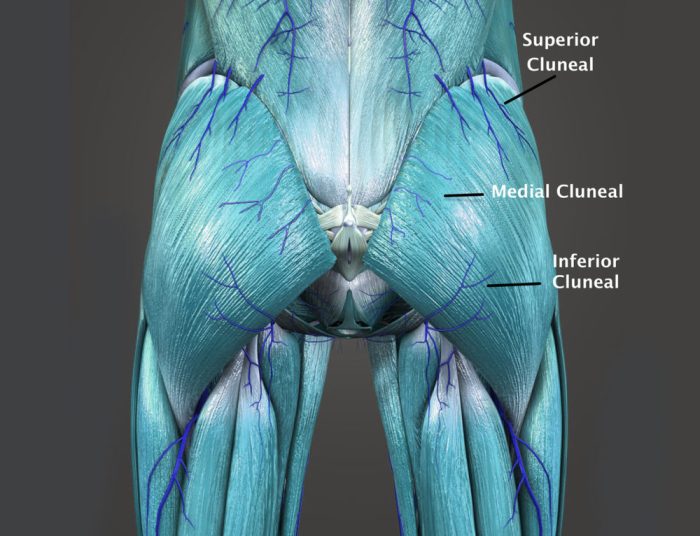
Anatomy and Function of Cluneal Nerves
The cluneal nerves are branches of the sacral plexus, a network of nerves originating from the lower spine. They are categorized into superior, middle, and inferior cluneal nerves, each supplying sensory information to specific areas of the buttock and lower back. The superior cluneal nerve primarily provides sensation to the upper buttock, the middle cluneal nerve to the mid-buttock, and the inferior cluneal nerve to the lower buttock.
Damage or irritation to any of these nerves can lead to localized or radiating pain.
Types of Cluneal Nerve Pain
Cluneal nerve pain manifests in various forms, each potentially linked to different underlying causes. Common types include sharp, shooting pain, a dull ache, or a burning sensation. The intensity and location of the pain can vary significantly depending on the affected nerve and the contributing factors.
Causes of Cluneal Nerve Pain: Mechanical vs. Non-Mechanical
Cluneal nerve pain can arise from both mechanical and non-mechanical sources. Mechanical causes typically involve direct pressure or trauma to the nerves, such as from poorly fitting clothing, prolonged sitting, or forceful impacts. Non-mechanical causes might involve conditions like inflammation, infections, or underlying medical issues.
Risk Factors for Cluneal Nerve Pain
Several factors increase the susceptibility to cluneal nerve pain. These include prolonged periods of sitting, repetitive movements, obesity, poor posture, and certain medical conditions. Individuals with pre-existing back problems or those engaging in physically demanding activities are also at a higher risk. Furthermore, individuals who frequently wear tight or ill-fitting clothing may experience increased pressure on the nerves, potentially leading to pain.
Comparison of Cluneal Nerve Pain Types
| Pain Type | Potential Causes | Characteristics | Symptoms |
|---|---|---|---|
| Sharp, shooting pain | Sudden trauma, muscle spasms, nerve compression | Intense, localized pain, often described as a “stabbing” or “electric shock” sensation | Localized pain, potentially radiating to surrounding areas, aggravated by movement. |
| Dull, aching pain | Prolonged pressure, inflammation, underlying conditions | Persistent, low-grade discomfort, often described as a “soreness” or “numbness”. | Generalized aching sensation in the buttock area, often worsened by rest or prolonged activity. |
| Burning sensation | Inflammation, nerve entrapment, irritation | Pain that feels like a burning or tingling sensation, often described as “hot”. | Localized or radiating pain, accompanied by a feeling of warmth or tingling. |
| Numbness/tingling | Nerve compression, diabetes, other systemic conditions | Loss of sensation, often described as “pins and needles”, can be associated with other symptoms. | Decreased or absent sensation in the affected area, often accompanied by a tingling or prickling sensation. |
Diagnostic Approaches
Unraveling the source of cluneal nerve pain requires a systematic approach, combining meticulous physical examination with appropriate imaging techniques. Accurate diagnosis is crucial for developing a personalized treatment plan and achieving optimal outcomes. A comprehensive diagnostic evaluation helps differentiate between various potential causes, ensuring the most effective interventions are implemented.Thorough diagnostic methods provide a pathway to understanding the underlying mechanisms contributing to cluneal nerve pain.
This understanding guides targeted interventions, promoting healing and restoring function. The diagnostic process aims to identify the specific trigger for the pain, allowing for tailored and effective treatments.
Physical Examination
A comprehensive physical examination plays a pivotal role in evaluating the cluneal nerve area. It involves a systematic assessment of the affected region, looking for any visible abnormalities or signs of inflammation. This includes inspecting the skin for lesions, redness, or swelling, and checking for any tenderness or muscle spasms.The examination proceeds with palpation, carefully feeling the tissues surrounding the nerve to identify any pressure points or areas of tenderness.
Careful attention is paid to the muscles of the back and buttocks, assessing for any tightness or spasms that might be contributing to the pain. Range of motion assessments are crucial to identify limitations in movement that might be related to nerve impingement or muscle stiffness. Neurological testing evaluates reflexes and sensation in the affected area. These tests help determine if nerve damage or compression is present.
Imaging Tests, How to release cluneal nerve pain
Various imaging techniques are available to visualize the cluneal nerve region and surrounding structures. These tests aid in identifying potential causes of the pain, such as herniated discs, bone spurs, or tumors. Different imaging modalities provide varying levels of detail and information.Magnetic Resonance Imaging (MRI) is a powerful tool for visualizing soft tissues like nerves, muscles, and ligaments.
It provides detailed images of the cluneal nerve and surrounding structures, offering insights into potential sources of compression or inflammation. Computed Tomography (CT) scans offer cross-sectional views of the body, including the spine and surrounding tissues. CT scans are useful in evaluating bony structures and identifying potential fractures or bony abnormalities. X-rays provide basic images of bones and joints, allowing for the detection of fractures, dislocations, or other skeletal abnormalities.
Diagnostic Tools Comparison
| Diagnostic Tool | Accuracy Rate | Limitations | Specific Applications |
|---|---|---|---|
| MRI | High | May be expensive; can be time-consuming | Identifying soft tissue abnormalities, nerve impingement, disc herniations. |
| CT Scan | High for bony structures | Less detailed view of soft tissues; potential exposure to radiation. | Evaluating bony structures, identifying fractures, and assessing the spinal canal. |
| X-ray | Moderate for skeletal issues | Limited view of soft tissues; not as detailed as MRI or CT. | Assessing fractures, dislocations, and other skeletal abnormalities. |
| Physical Examination | Moderate | Subjectivity in assessment; may not detect subtle abnormalities. | Identifying initial pain locations, muscle tension, and range of motion issues. |
Careful consideration of each diagnostic tool’s strengths and weaknesses is crucial for selecting the most appropriate method for a specific patient. The accuracy rates and limitations of each technique should be considered in the context of the individual patient’s clinical presentation. The selection of diagnostic tools should be guided by a clinician’s judgment based on the patient’s symptoms, medical history, and physical examination findings.
Non-Surgical Management Strategies
Relieving cluneal nerve pain often involves a multifaceted approach that focuses on managing the underlying cause and alleviating symptoms. Non-surgical methods offer a pathway to recovery, providing effective strategies without the need for invasive procedures. This approach emphasizes patient well-being and empowers individuals to take an active role in their healing journey.Effective non-surgical management often combines lifestyle adjustments, targeted physical therapy, and the strategic use of over-the-counter medications and topical creams.
A personalized plan tailored to individual needs and pain levels is crucial for optimal results. Understanding the various options available empowers patients to work collaboratively with healthcare professionals to achieve lasting relief.
Lifestyle Modifications
Lifestyle modifications play a significant role in managing cluneal nerve pain. Adopting healthy habits can help reduce inflammation and promote nerve healing. These modifications can significantly impact pain levels and overall well-being.
- Maintaining a healthy weight can reduce stress on the nerves and surrounding tissues.
- Regular exercise, such as walking or swimming, can improve circulation and flexibility, reducing pain and stiffness.
- Proper posture and ergonomics, especially when sitting or standing for prolonged periods, can prevent further nerve irritation.
- Avoiding activities that exacerbate pain, such as prolonged sitting or specific movements, is vital in the initial stages of pain management.
- Stress management techniques, such as meditation or deep breathing exercises, can help reduce muscle tension and inflammation.
Physical Therapy Exercises
Specific physical therapy exercises can strengthen muscles, improve flexibility, and promote nerve healing. A structured exercise program, tailored to individual needs, can contribute to pain relief and functional recovery.
| Exercise Type | Benefits | Contraindications | Examples |
|---|---|---|---|
| Gentle stretching | Improves flexibility and reduces muscle tension around the affected area. | Severe pain or inflammation in the initial stages. | Hamstring stretches, hip flexor stretches. |
| Strengthening exercises | Builds core strength and supports the back, reducing pressure on the nerves. | Severe pain or inflammation in the initial stages. | Plank variations, pelvic tilts. |
| Balance exercises | Improves stability and reduces the risk of falls. | Unstable or unsteady conditions. | Single leg stands, heel-to-toe walks. |
| Low-impact cardio | Enhances circulation, reduces inflammation, and improves overall well-being. | Severe pain or inflammation in the initial stages. | Swimming, stationary cycling. |
Over-the-Counter Pain Relievers
Over-the-counter pain relievers can help manage pain and inflammation associated with cluneal nerve pain. Selecting appropriate options depends on individual tolerance and potential side effects.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, can reduce inflammation and pain.
- Acetaminophen (paracetamol) can provide pain relief without the anti-inflammatory effects of NSAIDs.
- Always follow the recommended dosage instructions and consult a healthcare professional if side effects arise.
Topical Creams and Gels
Topical creams and gels can provide localized pain relief by reducing inflammation and promoting nerve function. They can offer alternative or complementary pain management strategies.
- Capsaicin creams, containing capsaicin, help desensitize nerve endings.
- Menthol and other cooling agents can offer temporary relief by numbing the affected area.
- Always test any topical cream on a small area first to check for allergic reactions.
Surgical Interventions (If Applicable): How To Release Cluneal Nerve Pain
Surgical intervention for cluneal nerve pain is a last resort, typically considered only after conservative treatments have failed to provide substantial relief. This approach aims to directly address the source of the pain and restore normal function, offering a potential path to lasting improvement for those who have not found relief through other means. Careful consideration of the risks and benefits, coupled with a thorough understanding of the individual’s medical history and specific condition, is paramount in making this decision.Surgical interventions for cluneal nerve pain are tailored to the underlying cause and location of the pain.
Different procedures may be employed depending on the specific diagnosis and the individual patient’s anatomy. These procedures may involve nerve decompression, removal of the source of irritation, or stabilization of the affected area. Successful outcomes hinge on meticulous surgical technique and the surgeon’s expertise in addressing the precise issue causing the pain.
Surgical Procedures for Cluneal Nerve Pain Relief
Surgical procedures for cluneal nerve pain aim to alleviate the compression or irritation of the nerve. This may involve a variety of techniques, including releasing pressure on the nerve from surrounding tissues, such as scar tissue or muscle hypertrophy, or removing the source of the irritation. The most common approach involves surgical decompression, carefully separating the nerve from the structures that are putting pressure on it.
Specific Situations Requiring Surgical Intervention
Surgical intervention for cluneal nerve pain might be considered in cases where conservative treatments, such as physical therapy, medication, and injections, have proven ineffective. Persistent and severe pain that significantly impacts daily activities and quality of life, along with nerve damage confirmed by diagnostic imaging and nerve conduction studies, may indicate a need for surgical intervention. In cases of tumors or other structural abnormalities compressing the nerve, surgical removal or decompression might be necessary.
Furthermore, if the nerve is trapped in a chronic, unremitting condition, surgery might be the most effective solution.
Potential Risks and Benefits of Surgical Procedures
Surgical procedures for cluneal nerve pain, like any surgical intervention, carry potential risks. These may include infection, bleeding, nerve damage, and persistent pain. However, the potential benefits of successful surgery can include significant pain relief, improved mobility, and enhanced quality of life. A thorough discussion with a healthcare professional will help weigh these potential risks and benefits and determine if surgery is the most appropriate course of action.
Factors like the severity of the pain, the patient’s overall health, and the experience of the surgical team all play a role in the decision-making process.
Step-by-Step Description of a Common Surgical Procedure
A common surgical procedure for cluneal nerve pain involves nerve decompression. The surgeon makes an incision over the affected area, carefully dissecting the surrounding tissues to identify and isolate the cluneal nerve. Structures compressing the nerve are then identified and released, ensuring the nerve is no longer subjected to pressure. The incision is closed, and the patient is monitored post-operatively.
The surgical technique will vary depending on the specific cause of the nerve compression and the patient’s anatomy. The post-operative recovery period is crucial for successful outcomes and may involve pain management, physical therapy, and careful monitoring.
Comparison of Surgical Approaches
| Surgical Approach | Description | Potential Benefits | Potential Risks |
|---|---|---|---|
| Nerve Decompression | Releasing pressure on the nerve from surrounding tissues | Significant pain relief, improved mobility | Infection, bleeding, nerve damage, persistent pain |
| Neurolysis | Destruction of the compressed nerve or surrounding tissue | Possible long-term pain relief | Potential for nerve damage, pain recurrence |
| Surgical Removal of the Source of Irritation | Removal of the source of irritation causing nerve compression (e.g., tumor, cyst) | Addressing the root cause, potentially complete pain relief | Risk of complications associated with the specific source removal, bleeding, infection |
Pain Management Techniques
Managing cluneal nerve pain effectively often involves a multifaceted approach, combining various strategies to address the root cause and alleviate symptoms. A personalized plan, tailored to individual needs and preferences, is crucial for optimal outcomes. This approach recognizes that pain is a complex experience, and different techniques can have varying degrees of effectiveness for different individuals.Effective pain management for cluneal nerve pain acknowledges the importance of addressing not only the physical discomfort but also the emotional and psychological aspects of the experience.
This holistic approach can significantly enhance the overall well-being of the patient.
Alternative Therapies
Alternative therapies offer a range of potential benefits for managing cluneal nerve pain. They can complement conventional treatments, offering alternative avenues for symptom relief and overall well-being. While some alternative therapies have demonstrated potential benefits in clinical studies, it’s essential to consult with a healthcare professional before incorporating them into your pain management plan. It’s important to note that the effectiveness of these therapies can vary significantly from person to person.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Advocates suggest that acupuncture can stimulate the nervous system, releasing endorphins, and reducing pain perception. However, the scientific evidence supporting acupuncture’s effectiveness for cluneal nerve pain remains somewhat limited. Some individuals report significant pain relief, while others experience minimal or no improvement.
- Massage Therapy: Manual manipulation of soft tissues, such as muscles and connective tissues, can help alleviate tension and improve blood flow to the affected area. Massage therapy may be particularly helpful in reducing muscle spasms and improving flexibility, contributing to a reduction in pain. The specific type of massage, such as deep tissue massage, can be tailored to the individual’s needs and preferences.
- Yoga and Tai Chi: These practices combine physical postures, breathing techniques, and meditation to improve flexibility, balance, and overall well-being. Yoga and Tai Chi can promote relaxation, reduce stress, and strengthen muscles, potentially leading to a decrease in pain. A properly guided and structured yoga or Tai Chi program can be very beneficial for managing chronic pain conditions.
- Herbal Remedies: Certain herbs, such as ginger or turmeric, have been traditionally used for pain relief. However, the effectiveness of herbal remedies for cluneal nerve pain is not always supported by rigorous scientific research. The use of herbal remedies should be discussed with a healthcare professional, particularly regarding potential drug interactions or side effects.
Relaxation Techniques
Relaxation techniques can be powerful tools for managing cluneal nerve pain. They work by reducing stress and muscle tension, which can contribute to pain reduction. These techniques can be practiced independently or combined with other therapies for enhanced results.
- Mindfulness Meditation: This practice involves focusing on the present moment without judgment. Mindfulness meditation can help reduce stress and improve emotional regulation, which can contribute to a reduction in pain perception. The practice of mindfulness has shown promise in reducing pain in several clinical studies.
- Progressive Muscle Relaxation: This technique involves systematically tensing and relaxing different muscle groups in the body. By consciously relaxing muscles, tension and pain can be reduced. The technique can be tailored to address specific areas of discomfort related to cluneal nerve pain.
- Deep Breathing Exercises: Consciously controlling breath can activate the parasympathetic nervous system, promoting relaxation and reducing the body’s stress response. This can have a positive impact on pain perception and overall well-being. Regular practice of deep breathing exercises can be beneficial for pain management.
Pain Management Techniques Comparison
| Technique | Potential Benefits | Potential Drawbacks | Additional Considerations |
|---|---|---|---|
| Acupuncture | Potential pain reduction, stress reduction | Potential for bruising or infection at insertion sites, limited scientific evidence | Consult with a licensed acupuncturist |
| Massage Therapy | Muscle relaxation, improved blood flow, reduced tension | Potential for discomfort during treatment, not a cure | Choose a qualified massage therapist specializing in musculoskeletal pain |
| Yoga/Tai Chi | Improved flexibility, balance, stress reduction | Requires dedication and practice, may not be suitable for all individuals | Enroll in a structured class for guidance |
| Herbal Remedies | Potential pain relief | Potential drug interactions, lack of rigorous scientific evidence, safety concerns | Consult with a healthcare professional before use |
| Mindfulness Meditation | Stress reduction, improved emotional regulation | Requires practice and patience, may not be effective for everyone | Guided meditation apps can be helpful |
| Progressive Muscle Relaxation | Muscle relaxation, reduced tension | Requires practice, may not be effective for everyone | Practice regularly for optimal results |
| Deep Breathing Exercises | Stress reduction, relaxation, improved well-being | Requires practice, may not be effective for everyone | Can be incorporated into daily routine |
Self-Care and Prevention

Taking proactive steps to prevent cluneal nerve pain is crucial for long-term well-being. By understanding potential triggers and implementing preventative measures, you can significantly reduce your risk of experiencing this discomfort. This section provides practical strategies to empower you in managing your health and fostering a pain-free life.
Identifying Potential Triggers
Recognizing and avoiding potential triggers is a vital aspect of preventing cluneal nerve pain. These triggers can range from prolonged sitting to specific types of footwear. Understanding your individual sensitivities is key to proactive pain management. Pay close attention to activities or situations that seem to exacerbate your pain. Maintaining a detailed pain journal can help identify patterns and pinpoint potential triggers.
Avoiding Triggers
Identifying triggers is the first step. The next is actively avoiding or minimizing exposure to those triggers. This could involve modifying your seating posture, choosing supportive footwear, or adjusting your daily activities to reduce strain on the nerve. Proactive measures to avoid triggers are essential for preventing further discomfort. Consistent avoidance helps minimize pain and discomfort.
Self-Care Measures for Alleviation
Implementing self-care measures can significantly alleviate cluneal nerve pain symptoms. These measures can include gentle stretching, applying cold or heat packs, and using over-the-counter pain relievers as needed. Consistency in these self-care routines can help manage symptoms effectively and improve overall comfort. Self-care measures should be tailored to individual needs and preferences.
Maintaining Good Posture and Body Mechanics
Maintaining proper posture and body mechanics plays a pivotal role in preventing cluneal nerve pain. Poor posture can put undue stress on the nerves in the lower back, potentially contributing to discomfort. Maintaining good posture and body mechanics is crucial for overall health and well-being. Simple adjustments in daily activities, such as maintaining an upright posture while sitting, can greatly reduce strain on the nerves.
Preventative Measures Table
| Preventative Measure | Effectiveness | Implementation Examples | Potential Benefits |
|---|---|---|---|
| Regular Stretching | High | Gentle hamstring and hip stretches, focusing on the area around the buttocks. | Improved flexibility, reduced muscle tension, and increased blood flow to the affected area. |
| Maintaining Good Posture | High | Using a supportive chair with lumbar support, sitting upright with feet flat on the floor, and avoiding prolonged periods of slouching. | Reduced pressure on the cluneal nerve, minimized strain on the lower back. |
| Ergonomic Workstation Setup | Moderate to High | Adjusting chair height and desk position to maintain a neutral spine posture, using a footrest if needed. | Reduced pressure on the lower back, improved comfort during prolonged periods of sitting. |
| Choosing Supportive Footwear | Moderate | Selecting shoes with good arch support and cushioning, avoiding high heels, and choosing shoes appropriate for activities. | Reduced strain on the lower back and surrounding muscles, minimized pressure on the nerve. |
Long-Term Management
Embarking on a journey toward long-term well-being with cluneal nerve pain requires a proactive and supportive approach. This involves understanding the importance of ongoing care, consistent adherence to treatment plans, and anticipating potential complications. This proactive management empowers you to navigate the path to recovery and sustained comfort.
Importance of Ongoing Monitoring and Follow-up Care
Ongoing monitoring and follow-up care are crucial for effectively managing cluneal nerve pain. Regular check-ups allow healthcare professionals to assess the effectiveness of the current treatment plan and identify any emerging issues or changes in your condition. This proactive approach ensures that the treatment strategy remains optimized and addresses evolving needs.
Importance of Adhering to Treatment Plans
Consistent adherence to the prescribed treatment plan is essential for achieving positive outcomes. This includes taking medications as directed, performing exercises regularly, and making lifestyle modifications as recommended. Commitment to the treatment plan is a powerful tool in managing pain and fostering healing.
Need for Regular Check-ups and Adjustments to the Treatment Plan
Regular check-ups are not just about monitoring pain levels; they are about proactively adapting the treatment plan. As your body responds to treatment, adjustments might be necessary. Healthcare professionals can fine-tune the approach to optimize results and ensure long-term effectiveness. This adaptability is key to achieving lasting relief and preventing setbacks.
Potential Complications of Cluneal Nerve Pain
While cluneal nerve pain often responds well to treatment, potential complications exist. These include the development of chronic pain syndromes, the potential for nerve damage worsening, or the occurrence of other related health issues. Recognizing these potential complications allows for proactive management and early intervention.
Resources for Ongoing Support and Information
Accessing reliable resources can significantly aid in the long-term management of cluneal nerve pain. These resources include support groups, online forums, and reputable healthcare websites. These platforms offer opportunities for connecting with others experiencing similar challenges, sharing experiences, and gaining valuable insights.
Closing Notes
So, you’re dealing with cluneal nerve pain? This guide armed you with the knowledge and tools to take control. Remember, proper diagnosis and a personalized treatment plan are key. Don’t hesitate to seek professional help if needed. You’ve got this! Now go out there and crush that pain!
Detailed FAQs
What are some common causes of cluneal nerve pain besides injury?
Sometimes, cluneal nerve pain isn’t caused by a direct injury. It could stem from underlying conditions like arthritis, tumors, or infections. It’s always a good idea to see a doctor for a proper diagnosis.
How long does it typically take to see improvement with non-surgical treatments?
Results vary, but many people experience some improvement within a few weeks of starting non-surgical treatments like physical therapy and medication. Consistency is key, and it’s important to communicate with your doctor about your progress.
Are there any specific exercises I should avoid if I have cluneal nerve pain?
Definitely! Exercises that put excessive stress on your lower back or hips should be avoided. Your physical therapist can advise you on the appropriate exercises for your specific condition.
What are some lifestyle changes I can make to prevent cluneal nerve pain?
Maintaining good posture, exercising regularly, and avoiding prolonged periods of sitting or standing can help prevent cluneal nerve pain. Staying hydrated and eating a healthy diet can also contribute to overall well-being.
